Fresh or Frozen Embryo Transfer?
Embryo Transfer: This is the culmination of the IVF process and every effort leading to this point. The embryo transfer itself is a simple procedure that follows IVF and is often considered the simplest and final step of the process. Though a simple process in and of itself, there are many factors and decisions that will be had leading up to the anticipated transfer day. Let’s discuss them here:
Fresh or Frozen Embryo Transfer?
Many more people are undergoing frozen embryo transfer (FET). This has a lot to do with the increased use of PGT (preimplantation genetic testing), where embryos are biopsied then frozen while awaiting the results. Reproductive endocrinology and infertility (REI) provider also recommend a freeze-all cycle for patients who have a high response and are at risk for ovarian hyperstimulation syndrome (OHSS).
But what about patients who are not testing embryos or have a low risk for OHSS? Are they better suited for a fresh or a frozen embryo transfer?
The truth is - the data isn’t perfect. Randomized controlled trials from China on good prognosis patients (young age, low BMI, many embryos available) showed higher live birth rates in women with PCOS who underwent FET. They showed similar live birth rates in ovulatory women, but much lower rates of OHSS with a freeze-all cycle. However, both of these studies assessed transfer of day 3 embryos. The same group then looked at ovulatory women undergoing blastocyst transfer and demonstrated higher live births with FET. A recent retrospective study from Italy looked at cumulative live birth rates for fresh vs frozen transfer by number of eggs retrieved. Live birth rates were similar for fresh and frozen transfer when <10 eggs were retrieved, but were higher if 11-25 eggs were retrieved. This data may be skewed because those with more eggs will automatically have higher pregnancy rates, but it does beg the question - do high hormone levels in high responder cycles adversely affect the endometrium and as such, implantation? Some studies have supported this.
Importantly, these findings cannot be applied to older patients or those with poor response. Also, there may be a risk that an embryo does not survive the thaw in an FET (this is very rare: <2-5%). Time to pregnancy is longer with a freeze all cycle.
The decision to do a freeze-all cycle should be individualized, but the data is reassuring that we are not doing patients a disservice by offering this.
Here’s a video on what we’ve discussed about fresh vs frozen embryo transfer.
Natural or Programmed?
Natural cycle protocol - times your FET based on when you naturally ovulate. While natural cycle may suggest that no additional medication is need, there are modified natural cycles where an hCG shot is given to ensure ovulation occurs
Programmed (artificial) cycle protocol - like the name suggest, the timing of your FET will be programmed and you will likely know in advance when your FET will be. You will be given estrogen and progesterone to mimic your body’s cycle, which will help the endometrium thicken and become receptive for implantation post FET
Your REI provider will be able to tell you which protocol would be best for you based on your health and infertility history.
Number of Embryos to transfer?
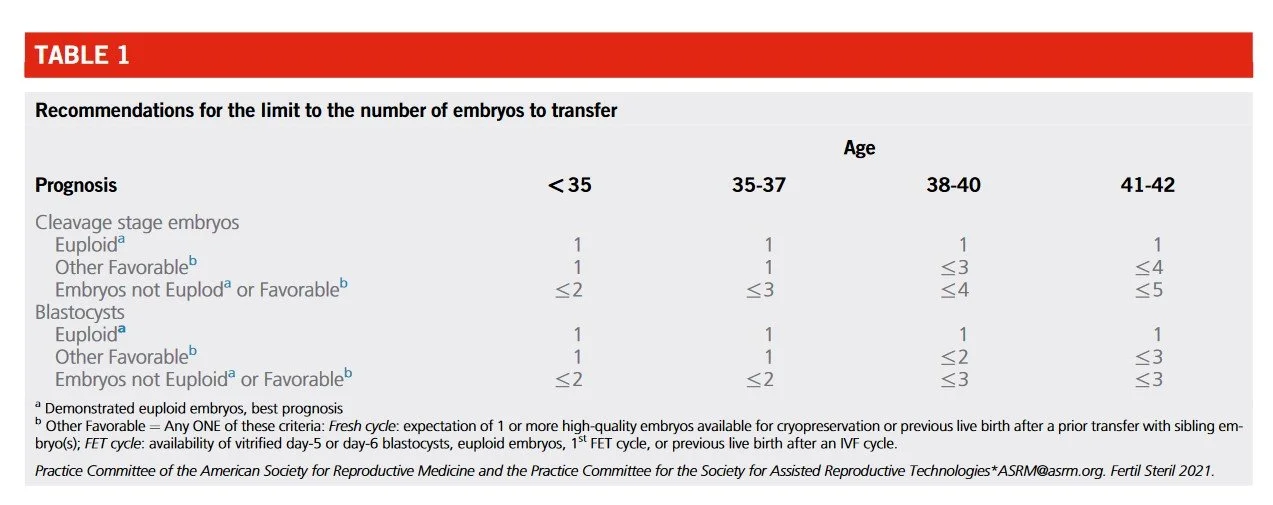
Recent guidance from the American Society for Reproductive Medicine (ASRM) recommend limiting the number of embryos to transfer due to the complications that comes with multiple pregnancies, and to limiting the number of embryos to transfer increase live birth rates. The number of embryos to transfer will be dependent on your age, embryo grade, and infertility history. See below for ASRM recommendations.
The numbers listed below the age category is referring to the number of embryo(s) to transfer based on age and prognosis
Sources for this article include:
Dr. Lucky Sekhon; Chen et al. NEJM 2016; Shi et al. NEJM 2018, Wei et al. Lancet 2019; Boynukalin et al. PLOS One 2020; Fertility and Sterility® Vol. 116, No. 3, September 2021.